What is a Refractive Lens Exchange (RLE)?
RLE is an intraocular lens replacement procedure in which the normal crystalline lens of the eye is exchanged with an intraocular implant. The implant has a specific power so that nearsightedness, farsightedness, and/or astigmatism can be corrected. The main goal of RLE is to reduce dependency on glasses and contact lenses.
Which patients are good candidates for RLE?
Patients with refractive errors that are either too high for laser vision correction, are over the age of 40 and desire improvement in both distance and reading vision, or those with early crystalline lens changes.
How safe is RLE?
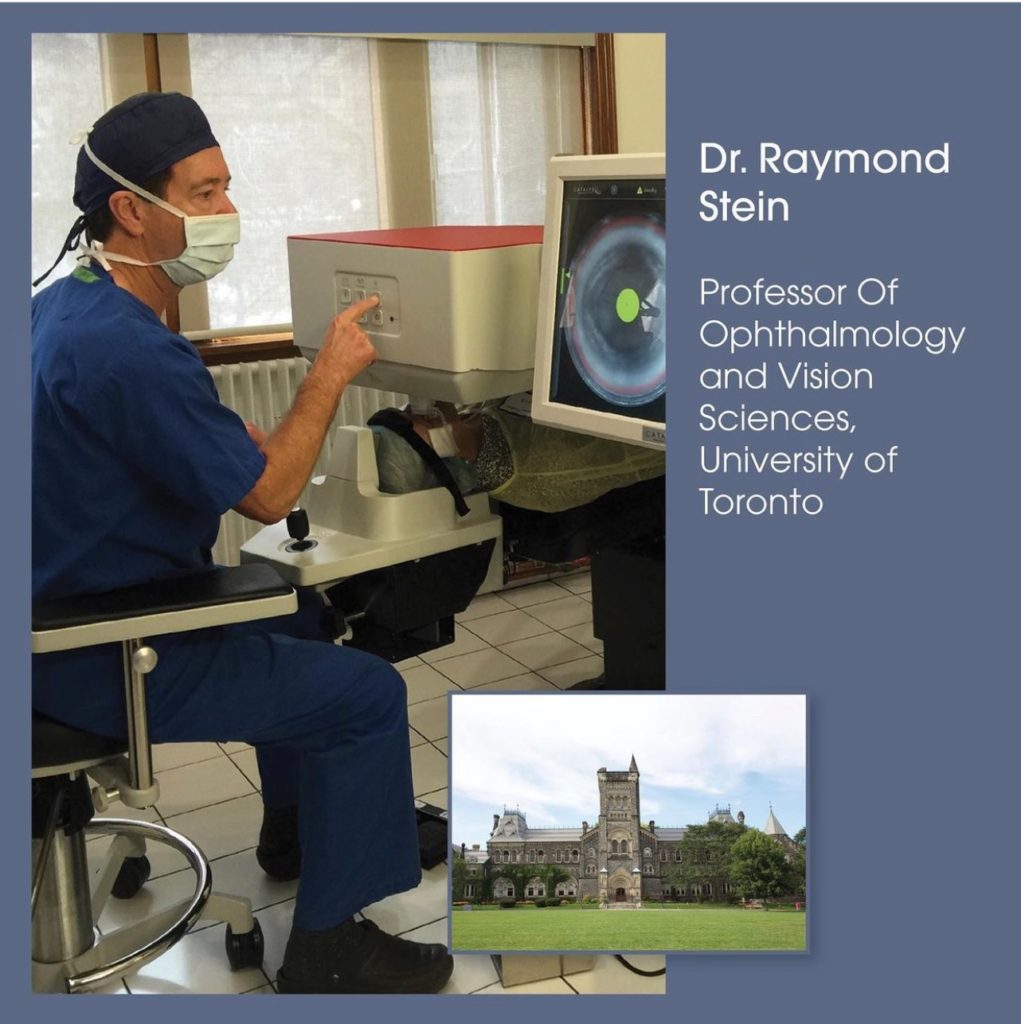
“RLE is a very successful operation. With a skilled surgeon using advanced technology patients usually have an excellent outcome.” says Dr Raymond Stein
Is the surgery painful?
No, in fact most patients are very comfortable during the procedure. There are no needles or sutures. The eye can be frozen with the simple application of anesthetic eye drops. Patients will notice a bright light from the microscope and a slight irritation but usually no discomfort.
Why does OHIP not cover RLE Surgery?
OHIP covers all medically necessary procedures. RLE surgery to reduce dependency on glasses or contact lenses is considered an elective procedure and not medically necessary.
Why do I require an implant at the time of RLE surgery?
After the lens is removed it is essential to have an implant, otherwise “coke-bottle” or extremely thick glasses are required in almost all patients. The lens normally helps to focus light on to the back of the eye for vision. An implant, with a specific power, will help to focus light and usually obviates the need for glasses or contact lenses.
How is the power of the implant determined?
The implant power can be determined by a variety of methods. The most accurate measurement is by the IOL Master, which uses a no-touch optical method to determine the length of the eye and the curvature of the front of the eye. Unlike with the older A scan method, no drops are required and nothing touches the eye. The information that is calculated is then inputted into a complex formula to determine the ideal power of the implant.
Are there different types of implants?
Yes, there are a number of different types of implants that can be used in RLE surgery. The main types of implants are aspheric, toric, and bifocal. An aspheric implant is a monofocal implant that is utilized when patients desire enhanced distance vision, and have low levels of astigmatism. A toric implant is the best choice in patients with higher degrees of astigmatism. The astigmatism correction of a toric implant is built directly into the implant and then the lens is rotated to a specific orientation in the eye. A bifocal implant is a multifocal implant that can provide both distance and near without glasses. There may be some glare and/or halos with this type of implant. These symptoms tend to diminish with time.
Are there any advantages to having RLE surgery at the Bochner Eye Institute versus a hospital?
The Bochner Eye Institute is one of the only independent eye surgical facilities outside of a hospital approved by the Ontario government. The surgeons are privileged to work with highly trained staff and utilize advanced RLE equipment. . There is no hospital in the Province that is able to offer the full range of elective choices. At the Bochner Eye Institute both Traditional RLE surgery and Laser RLE surgery are offered.
Is it advised not to wear makeup on the day of my surgery?
Yes, it is best not to wear any makeup on the day of surgery. We do not want any granules to enter the ocular surface or into the eye.
What clothes should I wear for my surgery?
Wear casual comfortable clothes. Do not have a tight collar shirt or sweater.
Can I eat prior to my RLE operation?
Yes, you can have light breakfast on the day of your RLE procedure.
What is used to clean my lids on the day of surgery?
A disinfectant is used to clean and disinfect the lids and surface of the eye. The solution is called Betadine. It has a brown colour and is very effective in preventing infection.
Will my face be covered with a drape?
A paper drape is placed over your head and body. You will have lots of room for proper breathing. There is an opening over your treated eye that allows the surgeon good visibility for the procedure.
If I am claustrophobic what can be done at the time of surgery?
The paper drape can be lifted up to a greater degree over your face. The anesthetist can give you either oral or intravenous sedation. The cataract procedure is very quick. Even the most claustrophobic patients tend to do well.
Can the anesthetist put me to sleep?
It is not necessary for you to be put to sleep. The procedure is relatively easy and quick for patients. Most patients find RLE surgery easier than having simple dental work. If you really feel you need some sedation this can be administered by the anesthetist.
What will I feel, see, and or hear during my operation?
At the very beginning of the operation you will see a bright light, which is the microscope light. You will then feel a slight burning or irritation, which is the intraocular anesthetic. After approximately 30 to 60 seconds the microscope light will be less intense. You will feel some slight pulling during the operation but no pain. You will hear an automated voice from the ultrasound machine that will sometimes speak words and other times make some noises like a symphony. After 10 to 15 minutes the operation will be over. When you sit up everything will have a red hue and be somewhat dark. This is simply a reaction to the bright light. The vision will gradually improve over 30 minutes.
Can both eyes be treated on the same day?
It is preferred to have each eye treated on a different day separated by a few days. Dr Stein wants to make sure the first eye is healing well before performing surgery on the other eye.
Do I need someone to take me home after my surgery?
It is important to have someone take you home after the procedure. You are not permitted to drive home yourself. We certainly want to make sure that you get home safely. If you have had some sedation you may be slightly drowsy.
What will my vision be like after surgery?
When you go home the vision will be slightly blurred. The vision is typically better within 24 hours, although it sometimes takes a few days for any transient corneal swelling to resolve. The vision tends to gradually improve over a few weeks.
What medications should I use after my surgery?
You will be given a prescription for two medications, a combination antibiotic and steroid drop, and a nonsteroidal anti-inflammatory drop, both to be used for 3 weeks.
When can I drive after my surgery?
You must get the green light from either your surgeon or your referring eye-care professional. Typically by the next day, after you see the doctor, you may be able to drive. However, it may take a while to get used to your new vision. You need to exercise caution when driving until you are used to your new vision.
What are the most common complications?
The most common complication is transient corneal edema. The cornea can respond to the ultrasound (i.e. phacoemulsification) with some swelling that typically resolves in a few days. Patients may have some irritation or foreign body sensation during the first few weeks from the micro incisions. Artificial tears or lubricating drops are usually helpful.
What is the chance of infection?
Infection is an extremely rare complication and occurs in less than 1 in 10,000 cases. The scientific name is endophthalmitis, which means infection in the eye. All precautions are taken to reduce the incidence of infection at the time of surgery including the use of an antibiotic placed inside the eye at the conclusion of the operation. If an infection occurs, intensive antibiotic drops are used. Occasionally, additional surgery is required to place additional antibiotics in the eye.
What is cystoid macular edema?
Cystoid macular edema is swelling of the back of the eye on the retina. This occurs with an incidence of 1 in 500 cases. The macular edema can affect vision but is treatable with nonsteroidal and steroid drops. Treatment is almost always successful in restoring vision.
Do I need to wear a protective shield at bedtime after surgery?
A protective shield is usually worn for 5 nights after surgery. The shield will protect the eye by preventing pressure on the eye when you are sleeping or from inadvertent rubbing.
When can I eat and drink after my surgery?
You can eat and drink as you normally would immediately after the surgery.
Should I restrict my activities after surgery?
The next day you can take a shower and shampoo your hair but try not to get water in your eye. Do not lift over 20 pounds during the first week after your operation. You may go for a walk and lift light weights at any time. Do not go swimming for 2 weeks after your surgery because of the risk of infection. If you are active with Yoga you can return within a week but do not stand on your head for 3 weeks.
What can I do if I am having difficulty reading immediately after surgery?
If you are having difficulty reading you can purchase a simple pair of reading glasses from the drug store or dollar store. Although they may not be ideal they will help you out until a proper pair can be prescribed. The eye is usually fully healed at 3 to 4 weeks from the surgery and this is the time that a new prescription can be prescribed if needed.
Will I require glasses after surgery?
Patients that have an aspheric or toric implant will usually only need glasses for reading. Patients that select a bifocal implant will typically not need glasses unless the print is very small or the lighting is poor.
What can I do if I find my vision is not really sharp after RLE?
Laser vision correction can be performed to enhance your vision. Although 95% of patients have clear vision after RLE, in some cases a small residual prescription may be present. In this situation, laser vision correction can be performed to refine your vision. There is no charge for the procedure. It is important that the eye is fully healed from the RLE and therefore we recommend waiting at least 3 to 4 months before having laser vision correction.
What can I do if I am experiencing irritation in my eye after surgery?
You can purchase an artificial tear at the drug store from the over-the counter section. There are a variety of excellent brands such as Systane Ultra, Systane Balance, Refresh, Genteal, and Blink. You can use the tear drop when needed anywhere from once to 4-5 time
Learn More about Raymond Stein
 Dr. Raymond Stein and his team are pleased to announce that Bochner Eye Institute is Toronto’s 2021 Top Choice Winner for Laser Vision Correction. The recognition honors “consistent excellence in the pursuit of customer satisfaction.”
Dr. Raymond Stein and his team are pleased to announce that Bochner Eye Institute is Toronto’s 2021 Top Choice Winner for Laser Vision Correction. The recognition honors “consistent excellence in the pursuit of customer satisfaction.”